PCSK9 Inhibitors: North Carolina
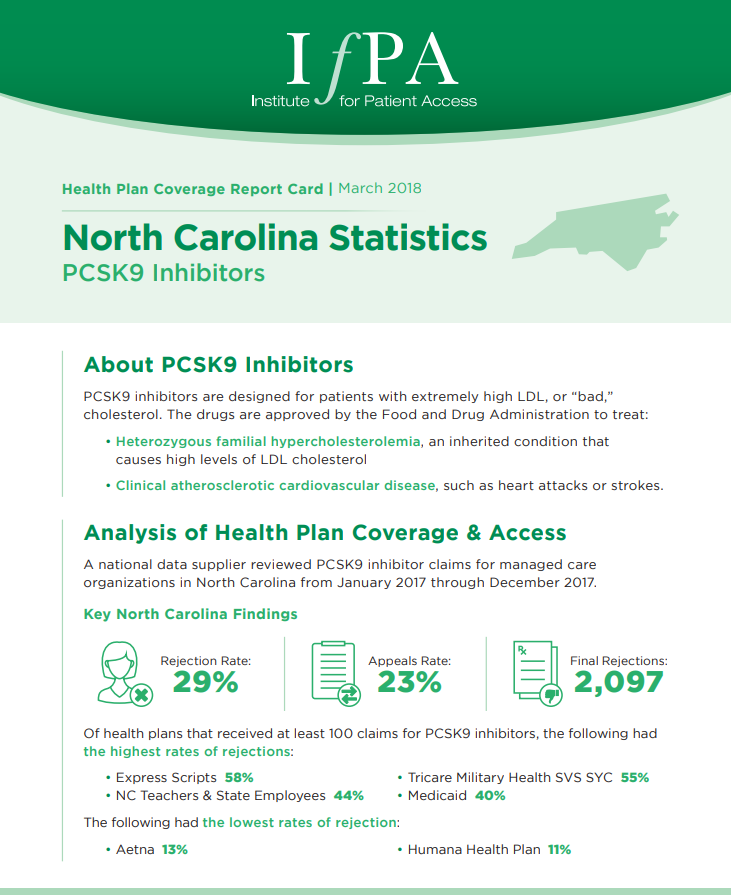
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in North Carolina from January 2017 through December 2017. Of health plans that received at least 100 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Express Scripts – 58% • Tricare Military Health SVS SYC – 55% • […]
PCSK9 Inhibitors: New York
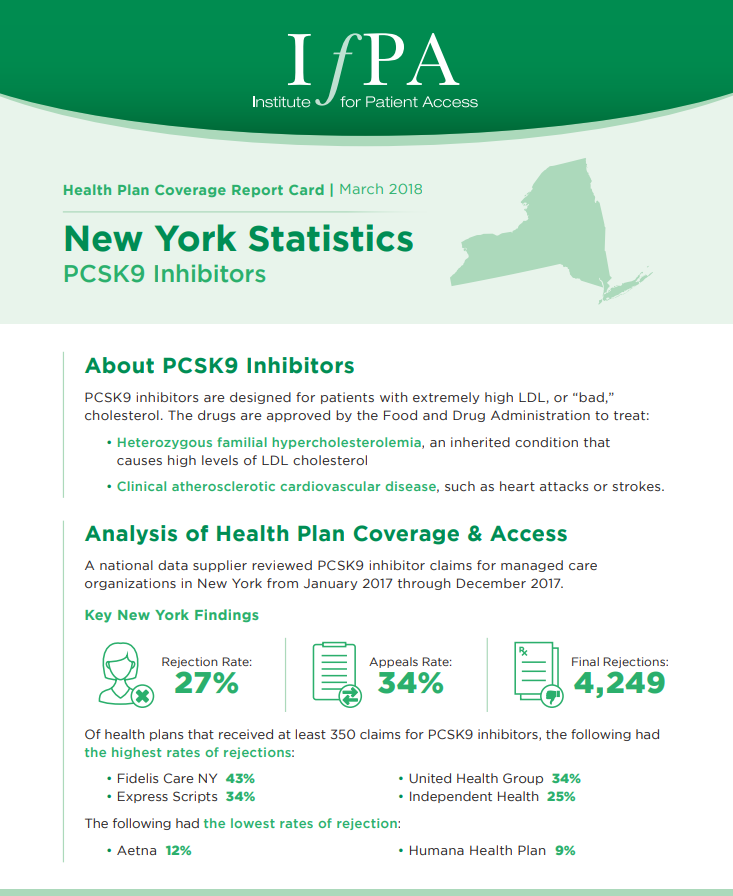
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in New York from January 2017 through December 2017. Of health plans that received at least 350 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Fidelis Care NY – 43% • United Health Group – 34% • Express […]
PCSK9 Inhibitors: New Jersey
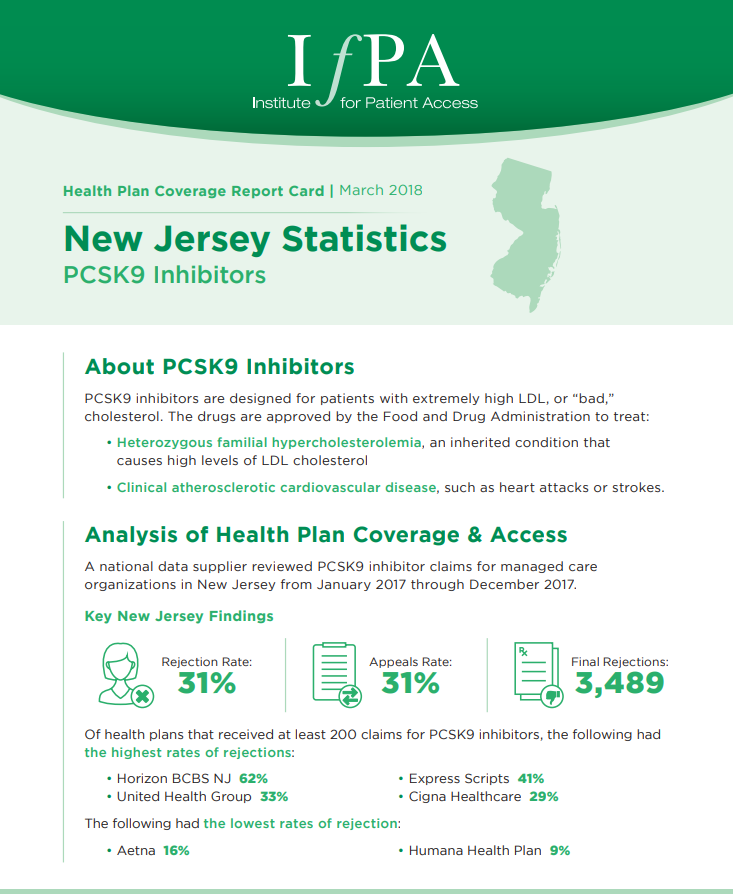
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in New Jersey from January 2017 through December 2017. Of health plans that received at least 200 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Horizon BCBS NJ – 62% • Express Scripts – 41% • United Health […]
PCSK9 Inhibitors: Mississippi
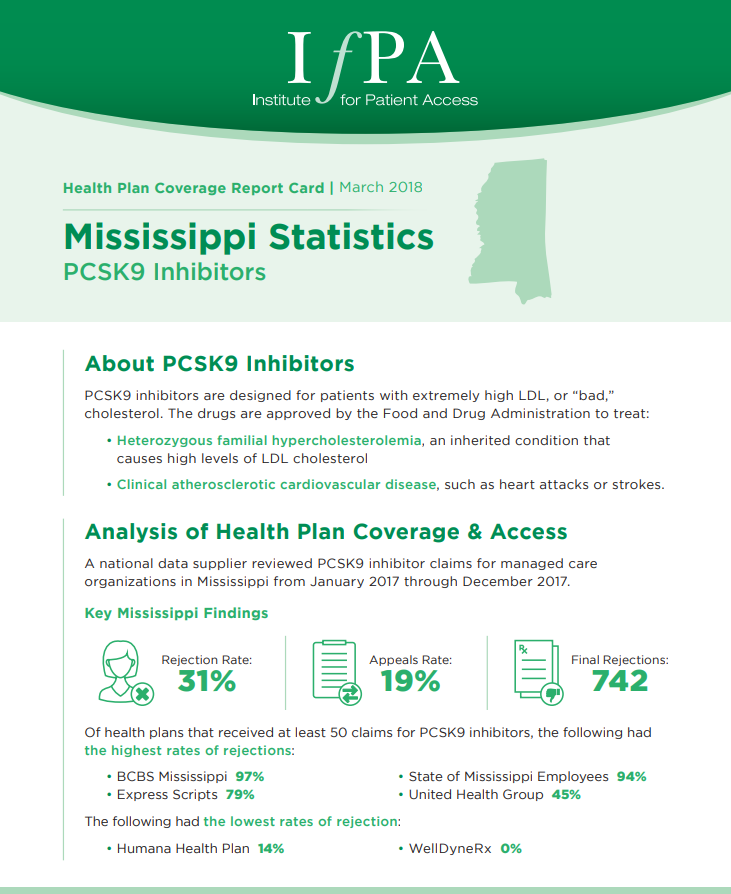
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in Mississippi from January 2017 through December 2017. Of health plans that received at least 50 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • BCBS Mississippi – 97% • State of Mississippi Employees – 94% • Express Scripts […]
PCSK9 Inhibitors: Indiana
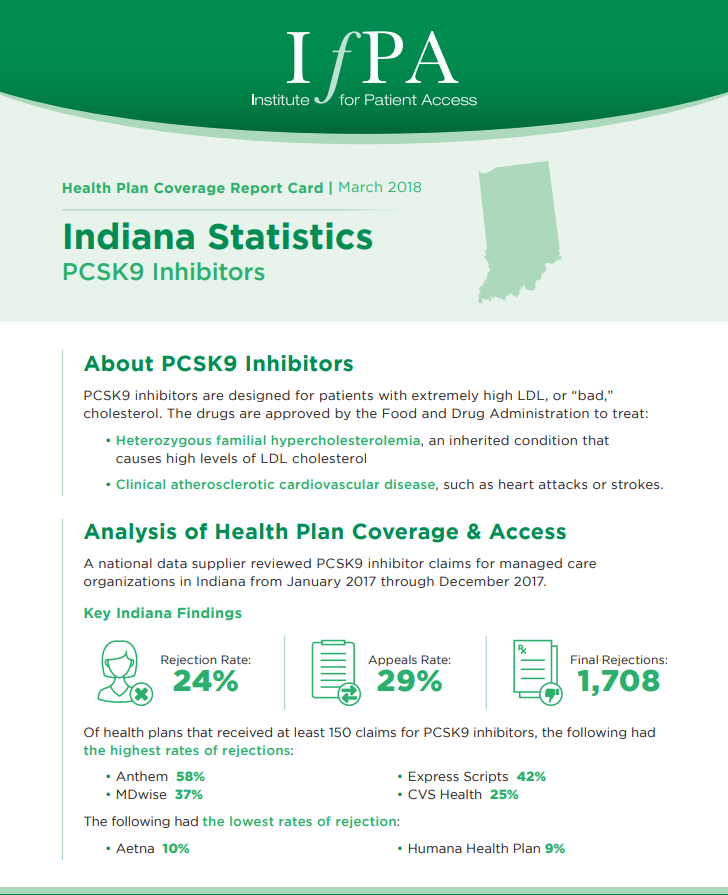
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in Indiana from January 2017 through December 2017. Of health plans that received at least 150 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Anthem – 58% • Express Scripts – 42% • MDwise – 37% • CVS […]
PCSK9 Inhibitors: Illinois
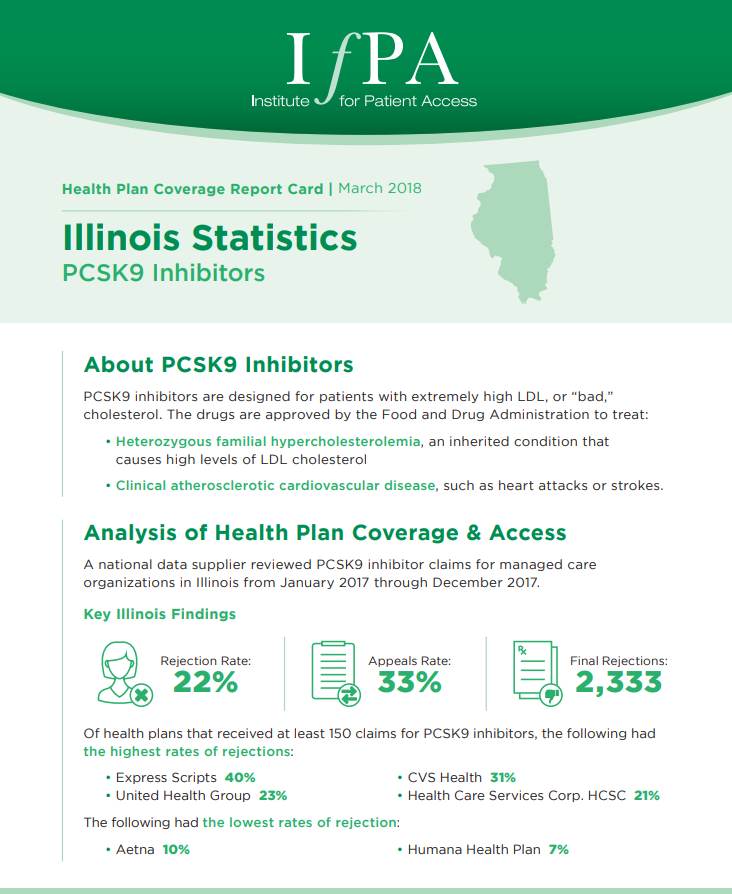
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in Illinois from January 2017 through December 2017. Of health plans that received at least 150 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Express Scripts – 40% • CVS Health – 31% • United Health Group – […]
PCSK9 Inhibitors: Georgia
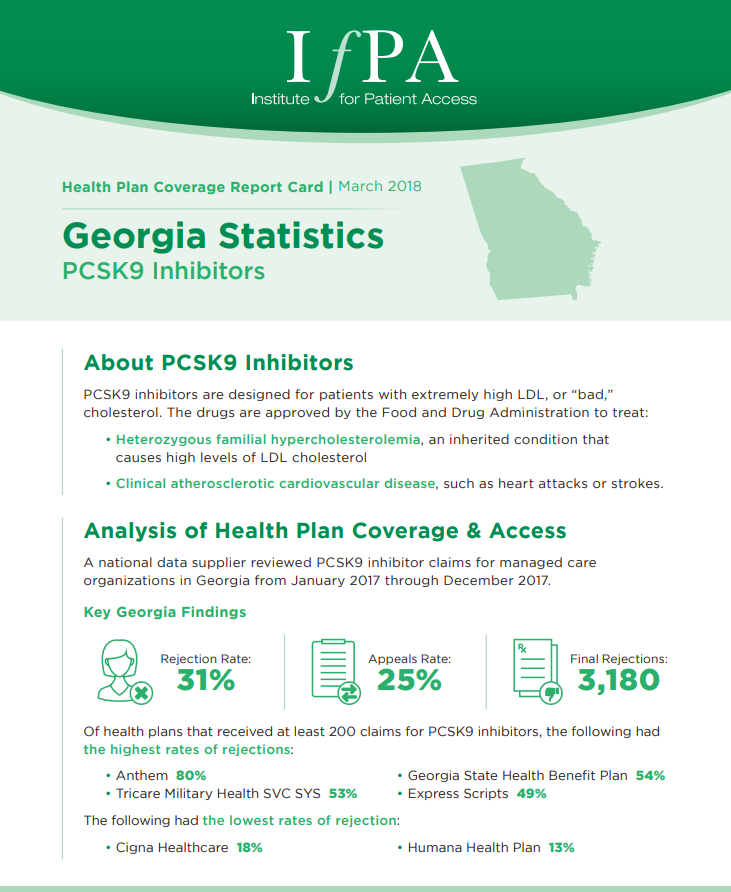
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in Georgia from January 2017 through December 2017. Of health plans that received at least 200 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Anthem – 80% • Georgia State Health Benefit Plan – 54% • Tricare Military […]
PCSK9 Inhibitors: Arkansas
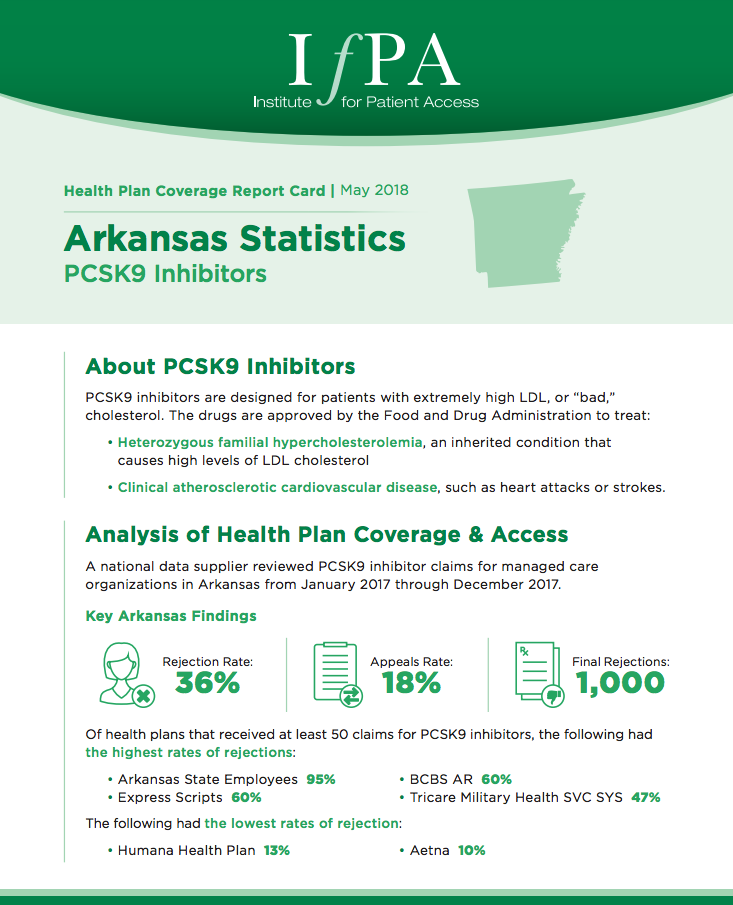
A national data supplier reviewed PCSK9 inhibitor claims for managed care organizations in Arkansas from January 2017 through December 2017. Of health plans that received at least 50 claims for PCSK9 inhibitors, the following had the highest rates of rejections: • Arkansas State Employees – 95% • BCBS AR – 60% • Express Scripts – […]
Research Confirms Prior Authorization Burden for Heart Patients

New research from the University of Pennsylvania details prior authorization requirements for PCSK9 inhibitors. The self-injected drugs lower bad cholesterol for patients with cardiovascular disease or genetic high cholesterol. Prior authorization allows health insurers to act as a gatekeeper, deciding whether they will cover the medication when it’s prescribed by a patient’s health care provider.
One Step Forward, Two Steps Back for Heart Patients
A money-back deal for cholesterol-lowering PCSK9 inhibitors doesn’t cut costs enough, claims a new analysis from a University of Pittsburgh researcher

