Health plans said “no” to one in every four Americans whose doctor prescribed a cholesterol-lowering PCSK9 inhibitor in 2017. And that, according to the Institute for Patient Access’ new access report cards, means that more than 78,000 heart patients went without medicine that could have reduced their risk of heart attack and stroke.
National Report Card Findings
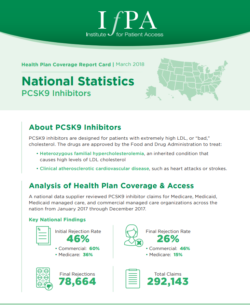 Report cards issued by IfPA capture claims information collected by a national data supplier between January and December of 2017. In its national report card, which reflects claims data from all 50 U.S. states, IfPA cites:
Report cards issued by IfPA capture claims information collected by a national data supplier between January and December of 2017. In its national report card, which reflects claims data from all 50 U.S. states, IfPA cites:
- 46% initial rejection rate
- 26% final rejection rate
- 78,664 PCSK9 inhibitor rejections nationwide.
The initial rejection rate reflects the scope of health plan prior authorization – which, physicians report, delay care for patients and take time from patient care.
The report card also pinpoints which health plans reject patients at the highest overall rates:
- Federal Employee Benefit Plan: 83%
- Tricare Military Health 49%
- Anthem: 45%
- Express Scripts: 38%
These plans also had among the highest rejection rates in last year’s national report card.
Overall rates combine data from commercial, Medicare, Medicaid and managed Medicaid plans.
Commercial vs. Medicare
This year’s national report card also isolates rejection rates for Medicare and commercial plans, revealing a disproportionately higher rate of rejection from commercial providers.
Commercial health plans had an average final rejection rate of 46 percent. Providers whose commercial plans rejected patients at a rate well above the national average included:
- Federal Employee Benefit Plan 83%
- Anthem 76%
- CVS Health 66%
- United Health Group 62%
By contrast, Medicare health plans had an average final rejection rate of 15%.
The Federal Employee Benefit Plan is a program through which insurance companies provide health benefits to civil servants and employees of the U.S. Government. Plan details can vary state to state.
The national plans ranked are those that processed at least 2,000 claims for PCSK9 inhibitors in 2017.
State Report Card Findings
IfPA has also issued report cards for 11 individual states, revealing final individual plan rejection rates as high as 97 percent, as with Blue Cross Blue Shield Shield of Mississippi. State report cards are available for:
- Alabama
- California
- Florida
- Georgia
- Illinois
- Indiana
- Mississippi
- New Jersey
- New York
- North Carolina
- Texas
Impact on Patients
Continued access barriers are “deeply troubling,” says Alliance for Patient Access Executive Director Brian Kennedy. “Health plans are using prior authorization to block tens of thousands of heart patients from the medication that their physician prescribed. These are patients who don’t respond adequately to traditional statins, yet health plans are cutting costs at their expense.”
Physician members of the Alliance for Patient Access’ Cardiovascular Disease Working Group have expressed frustration with the prior authorization process. In the group’s November 2016 white paper, Pamela Morris, MD, argues, “If providers prescribe PCSK9 inhibitors in accordance with the FDA-approved indications, patients should have access to the treatment.”
Partnership to Advance Cardiovascular Health Executive Director Ryan Gough echoed concerns about how national rejection trends impact patients. “While it’s encouraging to see modest progress since last year’s report cards, rejection rates are still far too high. Health plans may think they’re reducing costs, but leaving these patients vulnerable to stroke and heart attack ends up costing everybody.”
“We know that one American has a heart attack every 40 seconds,” Gough explained, adding “Fifteen percent of people who suffer a heart attack die from it. And heart attack is one of the most expensive hospital discharge diagnoses.”
Finally, the data suggest that rejections disproportionately impact patients employed through America’s armed services, government or civil service, AfPA’s Brian Kennedy noted. “Here you have patients who have dedicated their lives to public service, and they’re being denied their medication at twice the rate of the general population. It’s unconscionable.”
About PCSK9 Inhibitors
PCSK9 inhibitors block the PCSK9 protein from destroying a receptor on the liver that clears bad cholesterol. By prolonging the life of the receptor, the drugs increase the amount of LDL cholesterol that’s cleared from the body. Research shows that the drug allows some patients got their LDL levels down to as low as 19 and can reduce the risk of heart, stroke and cardiovascular death by 20 percent.
The therapies are approved for:
- Patients with a genetic predisposition toward high LDL cholesterol, known as familial hypercholesterolemia
- Those with atherosclerotic heart or blood vessel problems who don’t adequately respond to traditional treatments.

