What stands between patients and integrative, comprehensive pain management? It could be health plan design, according to a recent attitudinal survey by the Alliance for Balanced Pain Management.
The survey polled more than 300 health care professionals, patients, advocates and caregivers from across the United States. Overall, participants’ answers suggested that one-size-fits-all pain care persists largely because health plans don’t adequately cover more comprehensive, integrative approaches.
Key Findings
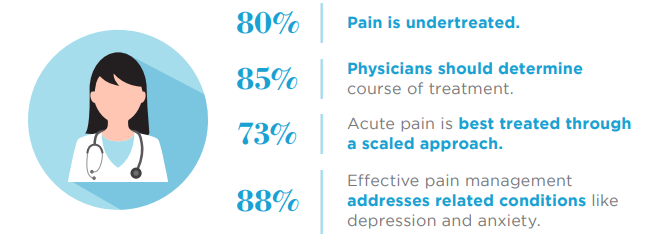
On the issue of approaches to pain management, respondents reported that:
- Pain is undertreated (80%)
- Physicians should determine course of treatment (85%)
- Effective pain management addresses related conditions such as anxiety and depression (88%).
Survey participants also weighed in on opioids, agreeing that:
- Limited coverage for integrative care forces patients to use opioids to manage their pain (60%)
- Abuse-deterrent opioids play a role in curbing the opioid crisis (62%)
- Overreliance on an opioid-only approach to pain has exacerbated the nation’s abuse and addiction problem (50%/plurality).
Finally, participants responded to statements about access to treatment, reporting that:
- Health plans don’t provide adequate coverage for integrative pain care (74%)
- Prior authorization unnecessarily blocks access to abuse-deterrent opioids (71%)
- Health plans should cover technology-based treatments and devices (74%).
Finding policy solutions that give physicians and patients more options to safely, effectively treat pain has long been a priority for the Alliance for Balanced Pain Management. The group issued a white paper earlier this year detailing five policy proposals for improving access to comprehensive, integrative pain care.
To learn more, see the Alliance for Balanced Pain Management’s full survey results.

